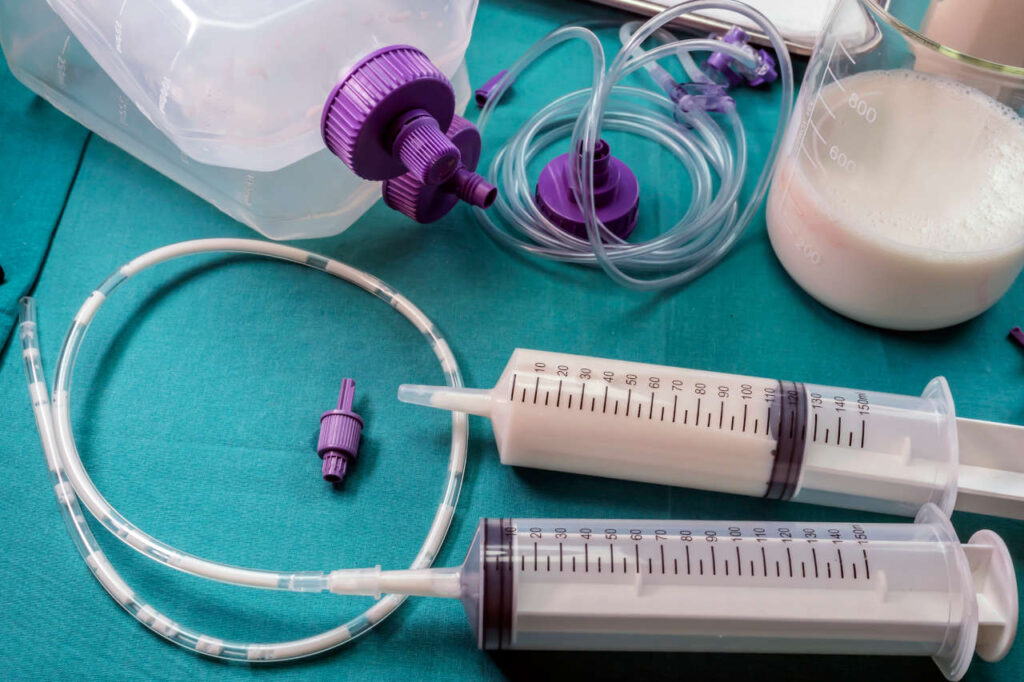
For patients who rely on enteral nutrition, managing medications through a feeding tube can be a complex but essential part of care. When done correctly, medication administration supports overall health, improves outcomes, and minimizes discomfort. With the growing availability of professional home healthcare, families opting for tube feeding at home in Dubai(التغذية الأنبوبية في المنزل في دبي) are increasingly seeking guidance on how to safely integrate medications into daily feeding routines. Understanding which medications are safe, how to administer them, and how to avoid tube blockages or reduced effectiveness is key to successful home-based care.
Why Medication Management Matters in Tube Feeding:
Feeding tubes are designed primarily for delivering nutrition and hydration. However, many patients also require daily medications for chronic or acute conditions. If these drugs are not properly prepared or administered through the tube, it can result in:
- Reduced drug effectiveness
- Adverse drug interactions
- Tube blockages or clogs
- Gastrointestinal discomfort
- Potential overdose or underdose
Caregivers and healthcare professionals must work together to tailor a plan that considers the patient’s full medication profile and tube feeding schedule.
Types of Feeding Tubes and Their Impact on Medication Delivery:
Not all tubes are the same. The location and type of feeding tube play a major role in how medications should be given:
Nasogastric (NG) Tubes:
- Inserted through the nose into the stomach
- Suitable for short-term use
- Accommodates most oral medications when crushed and diluted
Gastrostomy (G-Tube):
- Surgically placed into the stomach
- Common for long-term care and stable medication regimens
- Most versatile for administering blended meds and formula
Jejunostomy (J-Tube):
- Bypasses the stomach and feeds directly into the small intestine
- Absorption is faster but requires more caution
- Some medications may be less effective when not absorbed through the stomach
Best Practices for Administering Medication via Feeding Tube:
Proper preparation and timing make all the difference. Follow these essential steps for safe administration:
1. Consult a Pharmacist or Physician:
- Verify that each medication is safe for tube use
- Check if any meds should not be crushed or altered
- Get guidance on liquid alternatives or compounding options
2. Use Liquid Medications Whenever Possible:
- Ready-made suspensions are ideal for tube administration
- They reduce the risk of clogs and provide uniform dosing
- Ask for sugar-free and alcohol-free versions to minimize side effects
3. Crush and Dilute Solid Medications Correctly:
- Only crush tablets that are labeled as safe to do so
- Mix the crushed powder with at least 15–30 mL of warm water
- Avoid mixing multiple medications in one syringe
4. Flush the Tube Before and After Medications:
- Use 15–30 mL of water to flush before giving meds
- Repeat flushing between different medications
- Final flush ensures all residues are cleared from the tube
5. Separate Feeding and Medication Times:
- Pause tube feeding 30 minutes before and after administering meds
- This prevents interactions and improves absorption
- Resume feeding after all medications and flushes are completed
Medications That Should Never Be Crushed or Mixed:
Certain drug types should not be administered through a feeding tube unless specifically reformulated:
- Enteric-coated tablets: Designed to dissolve in the intestine, not the stomach
- Sustained-release or extended-release meds: Crushing alters the release mechanism, leading to overdose
- Cytotoxic drugs (e.g., chemotherapy): Risky for caregivers to handle and unsafe via feeding tubes
- Hormonal or highly irritating drugs: May cause inflammation or harm to mucosal linings
Ask your healthcare provider for alternative formulations or delivery methods when dealing with such medications.
Medication and Tube Interaction Risks:
Certain medications can negatively affect the feeding tube or interact with the formula itself:
- Phenytoin (anti-seizure medication): Binds with feeding formula, reducing effectiveness
- Antibiotics like ciprofloxacin: Absorption may be affected if given with formula
- Iron supplements: Can stain the tube or react with other drugs
- Sucralfate: Thickens and may cause clogs
To avoid interactions:
- Space out medication and formula administration
- Switch to intravenous delivery when absorption is critical
- Regularly check the tube for signs of buildup or blockage
Common Medication-Related Complications and Solutions:
Caregivers should remain alert to signs that medications are not being absorbed properly or are causing side effects:
Signs to Watch For:
- Sudden behavior or mood changes
- Nausea or vomiting post-medication
- Increased reflux or constipation
- Decreased medication effectiveness
- Resistance when flushing the tube
Solutions to Consider:
- Reassess the feeding and medication schedule
- Consult the prescribing doctor to change dosage or form
- Request a pharmacy review of all medications
- Increase hydration to flush residue more effectively
Role of Caregivers in Medication Management:
Whether family members or licensed nurses, caregivers are crucial in ensuring medication safety during tube feeding. Their responsibilities include:
- Maintaining an accurate medication chart
- Checking expiry dates and storage instructions
- Using gloves and hygiene protocols during administration
- Reporting any side effects to the healthcare team
- Keeping track of changes in behavior, digestion, or comfort
In Dubai, many caregivers working with tube feeding at home (التغذية الأنبوبية في المنزل)receive certified training from healthcare providers, ensuring they’re well-equipped for medication administration.
Tips for Organizing Medication Schedules at Home:
Managing multiple medications alongside nutrition feeds requires organization and consistency. Helpful strategies include:
- Medication timetable: Chart showing names, dosages, and times
- Color-coded syringes: Assign a different color for each med to avoid mix-ups
- Weekly pill organizers: For those with medications that can be pre-dosed
- Smartphone reminders or alarms: Prevent missed doses
- Label everything clearly: Including flush syringes, med syringes, and water containers
Consistency reduces risk and builds caregiver confidence.
Communication with the Healthcare Team:
Maintaining open communication with doctors, dietitians, and pharmacists is key to safe medication use. Share updates regularly about:
- New symptoms or reactions
- Difficulties in flushing the tube
- Any changes in the patient’s eating or hydration habits
- Adjustments to tube feeding formulas that could affect absorption
Using telemedicine or digital logs helps make this communication faster and more convenient.
Staying Updated on Medication Guidelines:
The medical field is constantly evolving, and guidelines for tube feeding and medication management are no exception. Stay informed through:
- Regular consultations with your pharmacist
- Online training modules for caregivers
- Updates from local health authorities
- Support groups for tube-feeding families
- In-home checkups from certified nurses or doctors
Being proactive helps prevent errors and keeps patients safer at home.
Final Thoughts:
Managing medications through a feeding tube requires precision, knowledge, and consistent care. When approached with the right information and planning, it becomes a safe and manageable part of home healthcare. For families embracing tube feeding at home in Dubai, understanding medication protocols enhances patient comfort, prevents complications, and ensures that both nutrition and treatment goals are met effectively.
With trained caregivers, medical oversight, and organized routines, medication administration can become a seamless part of daily care—empowering patients to heal and thrive within the comfort of their homes.